Back pain in the lumbar region is known to everyone. According to statistics, it is she who causes 25% of all medical requests. Its appearance can provoke many different factors, from mundane fatigue to quite serious illness. Therefore, you should not ignore the problem, especially if the discomfort occurs regularly and over time. In such situations, you should contact a therapist as soon as possible or contact a neurologist directly and undergo a full examination. This makes it possible to diagnose the disease at an early stage in its development and to take timely measures to stop its progression. However, if there was an injury or an unsuccessful fall on the eve of the onset of pain, you must immediately register for a consultation with a traumatologist or spinal surgeon.
This makes it possible to diagnose the disease at an early stage in its development and to take timely measures to stop its progression. However, if there was an injury or an unsuccessful fall on the eve of the onset of pain, you must immediately register for a consultation with a traumatologist or spinal surgeon.
Characteristics of back pain and accompanying symptoms
Back pain can be of different types and severity. They can be strong, shoot, whine, pull, etc. They may increase in strength with physical exertion, sitting or standing for long periods, and may or may not pass away at rest. All of these are important diagnostic factors that will allow the doctor to make the correct diagnosis and find the real cause of the patient's condition.
Of fundamental importance for the diagnosis is whether the pain is radiating to the hips, buttocks, knees, feet and if so, where and how. Another important factor is the presence of restrictions on the mobility of the spine, regardless of whether the patient can freely make bends, body rotations or restricted mobility.
Pain in the spine is known as lumbodynia. If it spreads to the legs, it is called lumboischialgia.
Acute pain lasts less than 3 months, otherwise it is called chronic pain. In the latter case, the disease often proceeds with periods of exacerbation and remission.
Lower back pain rarely occurs in isolation. In most cases, there is also a complex of other diseases that the patients themselves rarely associate with one another. Back pain is often combined with:
- Sensation of crawling in the back and / or legs, numbness;
- muscle weakness;
- pain in the hip, knee joints;
- Disorders of the pelvic organs (menstrual disorders, potency problems, loss of control when urinating, bowel movements);
- leg paralysis.
Similar signs indicate a pathology of the spine. However, since they can not only provoke the occurrence of back pain, there is another group of symptoms that are associated with lower back pain, which can indicate the pathology of internal organs or cancer. Therefore, you need to be extra careful with your own status when it appears:
However, since they can not only provoke the occurrence of back pain, there is another group of symptoms that are associated with lower back pain, which can indicate the pathology of internal organs or cancer. Therefore, you need to be extra careful with your own status when it appears:
- faster and unnecessary weight loss;
- cuts and pains in the groin, perineum;
- increased urination, pain;
- increase in body temperature, chills;
- changes in skin color in the area of the epicenter of pain;
- Menstrual irregularities, unusual discharge.
If lower back pain is associated with one or more of the above symptoms, you should seek medical attention immediately. If symptoms from the first group appear, then it is necessary to consult a neurologist, from the second group onwards, the help of a urologist, gynecologist, endocrinologist or other narrow specialist is necessary. The therapist will help you understand exactly which doctor to contact.
Causes of occurrence
All causes of back pain in the lumbar spine can be divided into two groups: diseases of the spine and diseases of the internal organs, especially gynecological diseases, diseases of the kidneys, organs of the gastrointestinal tract, endocrine diseases. Most often, however, they are a result of the development of changes in the spine and surrounding muscles. The most common causes of back pain are:
- osteochondrosis;
- spondylosis;
- inflammatory diseases of the spine;
- myofascial syndrome;
- ankylosing spondylitis;
- scoliosis;
- injuries.
However, back pain can also be attributed to overload or certain physiological changes. In such situations, they do not require special treatment, only a decrease in physical activity and a more frugal daily regimen.
Osteochondrosis and intervertebral hernias
Osteochondrosis is the most common disease of the spine. Its development is often associated with inevitable age-related changes, since almost every elderly person has their symptoms to a greater or lesser extent.
Osteochondrosis is mankind's price for being able to walk straight ahead. It is characterized by a gradual destruction of the intervertebral discs, their thinning, a decrease in elasticity and strength. As a result, they stop dealing with stress and can bulge. This is how intervertebral hernias develop.
Most often, osteochondrosis affects the intervertebral discs of the lumbar spine. When they protrude into the spinal canal or the foramina foraminalis, the nerves are almost inevitably compromised, which leads to acute pain in the lower back and their irradiation of the legs and buttocks.
Spondylosis
Spondylosis is a complication of advanced osteochondrosis in which the intervertebral discs are almost completely destroyed. Due to the ongoing degenerative processes and an increase in the load on the spine along the vertebral edges, bony protrusions, so-called osteophytes, form. Therefore, there is a high risk of compression and injury to neighboring nerves. This causes severe pain that can spread to the legs.
Therefore, there is a high risk of compression and injury to neighboring nerves. This causes severe pain that can spread to the legs.
Inflammatory diseases of the spine
The most common inflammatory diseases of the spine occur in young people and mainly in men. They cause severe pain, which is also disturbing at night, which is their specific difference. If there is no timely treatment, the pain will progressive and bother the person more often.
It is not uncommon for patients to seek medical help several years after the first symptoms appear. As a result of such a long course of the inflammatory process in the spine, irreversible changes can occur, which can ultimately lead to immobility and disability.
Sometimes, in addition to lower back pain, there are discomforts in the joints of the legs and arms. In such cases, the cause of discomfort can be arthritis or osteomyelitis.
Myofascial Syndrome
Myofascial syndrome is a common pathology in which pain occurs after a long stay in an uncomfortable position or after physical exertion. The myofascial syndrome occurs somewhat more frequently in women. Back pain occurs after careless movement or physical exertion. Its peculiarity is the presence of so-called trigger points on spasmodic muscles in the lumbar spine and in the buttocks, which lead to a sudden attack of pain. The myofascial syndrome significantly reduces the quality of life of humans, but does not pose a serious threat.
Bechterew's disease
Ankylosing spondylitis or ankylosing spondylitis is a chronic joint disease that mainly affects the sacroiliac joint, the joints of the spine and the surrounding soft tissues. With this disease, people are concerned about back pain, sacral pain and stiffness of movements, but symptoms usually go away without a trace in the afternoon and night.
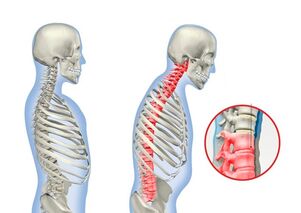
In addition, physical activity has a positive effect on the patient's well-being and helps to eliminate the pain syndrome. A specific symptom of ankylosing spondylitis is stooping, the arched curvature of the spine, and the progressive reduction in mobility.
Scoliosis
Scoliosis is a sideways curvature of the spine. It can be of varying degrees of severity, which directly affects the intensity of back pain and other symptoms. Since the deformation of the spine leads to a displacement of all anatomical structures, the nerves are often pinched, which leads to severe pain. Other neurological symptoms may also be present, including feelings of numbness and paresis.
Compression fractures
In the elderly with osteoporosis and trauma, lower back pain can be the result of an undetected compression fracture of the spine. As a result, the vertebrae are flattened and assume an abnormal position, which leads to a wrong distribution of the load on the spine, degenerative processes in the intervertebral discs and the appearance of pain.
Physiological causes of back pain
Intensive sports training leads to increased stress on the muscles during hard physical work, as a result of which lactic acid accumulates in them and causes pain. Back pain is not uncommon when wearing uncomfortable shoes for a long time, especially with heels.
Pain in the lower back is also often observed during pregnancy. In such situations, they are caused by a shift in the center of gravity and increased stress on the spine.
Diagnosis
It is recommended to consult a neurologist to determine the causes of back pain in the lumbar spine. Initially, you can seek advice from a therapist, but most likely the doctor will continue to refer the patient to a neurologist.
At the appointment, the specialist conducts a thorough interview with the patient to find out what worries him, what lifestyle he leads, etc. In addition, an examination is required in which the doctor assesses the severity of reflexes, performs neurological tests and theMobility of the patient assessed. Based on the results obtained, the doctor can make a preliminary diagnosis and understand what kind of violations led to the appearance of back pain and back pain.
In order to confirm the existing assumptions and to pinpoint the causes of the pain, a comprehensive examination of the patient is carried out, which may include:
- general and biochemical blood tests - with their help, changes in the blood are detected, which indicate inflammatory processes in the body, the presence of an infection or a tumor;
- general urinalysis - to distinguish kidney disease as a cause of pain in the lumbar region;
- X-ray - shows the presence of a change in the bone structures of the spine, signs of fractures, provides information about bone density and allows the diagnosis of serious diseases of the spine, as well as osteoporosis (the detection of pathologies of the spine is a reason for a more thorough examination using CTor MRI);
- CT is a modern method of radiation diagnostics with which you can visualize all bone structures very clearly and recognize the smallest deviations from the norm.
- MRI - provides comprehensive information on the condition of soft tissues and cartilage, including intervertebral discs. MRI can diagnose intervertebral hernias of any size, changes in blood vessels, and tumors.

Treatment of back pain
The treatment of back pain is selected strictly on an individual basis. At the same time, it is always complex and includes symptomatic therapy, lifestyle changes and treatments to eliminate the discovered causes of back pain. Therefore, if the first two components of therapy, as a rule, are universal and prescribed to all patients, then etiotropic therapy is developed strictly individually, taking into account the existing disease.
In most cases, patients are initially offered conservative treatment, the main component of which is drug treatment. In more complex cases, it is also recommended to take a course on physiotherapy, manual therapy and exercise therapy.
In any case, all patients with back pain should:
- Give up lifting heavy objects and doing sports.
- for weight loss in the case of obesity;
- take regular breaks to warm up when a person is forced to sit for a long time;
- increases physical activity, but avoids overload and hard work (daily walks, morning exercises, conducting a special movement therapy complex, swimming);
- Use a support bandage that takes pressure off the lower back and thus offers favorable conditions for the early restoration of the spine.
Depending on the source of pain, patients may be advised to stay in bed for a few days or, on the contrary, to increase their physical activity, but within reasonable limits. For example, pain caused by nerve compression requires you to rest your back for a few days. For other diseases, however, moderate physical activity is one of the mandatory components of therapy. It helps to increase the effectiveness of drug treatment, reduce the risk of complications, and prevent disability.
Unfortunately, conservative therapy cannot always be used to treat back pain. In some cases, it turns out to be ineffective and does not give results even after several months of unwavering adherence to medical recommendations. In other situations, the results of the examination reveal the presence of a pathology that can no longer be eliminated using non-surgical methods. In such situations, patients are advised to consult a neurosurgeon and perform appropriate surgical interventions to restore the normal anatomy of the spine.
drug therapy
To improve the patient's condition and quickly relieve pain, the following is prescribed:
- NSAIDs in the form of tablets, injections and topical preparations - have analgesic and anti-inflammatory properties;
- corticosteroids - in short courses to control severe inflammation;
- muscle relaxants - necessary to relieve muscle spasms, which are often a reflex reaction of the body to pain and make it worse;
- B vitamins - improve nerve conduction by normalizing the nutrition of nerve fibers and increasing the speed of transmission of nerve impulses.
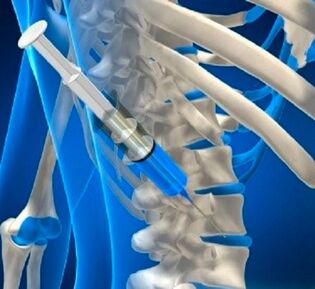
In the case of severe pain that cannot be tolerated, blockades can be carried out. The procedure involves injecting an anesthetic solution directly into the area of pain or the nerve fiber passage. Thus, for a while, it is possible to completely stop the pain syndrome and improve the patient's well-being.
However, the blockade has only a temporary effect, and its implementation is only possible in a medical facility, since most of the time the drug must be injected into places very close to the spine, where a mass of nerves passes. An illiterate implementation of the procedure can therefore have serious and sometimes fatal consequences.
In addition to the drugs listed above, a number of others are prescribed that will help eliminate the underlying disease that caused the pain syndrome. Therefore, patients can also be prescribed antibiotics, chondroprotectors, immunomodulators and drugs from other groups.
Physiotherapy
Physiotherapy treatments are often prescribed for patients with spinal disorders. Thanks to the correctly chosen method of physical manipulation and the frequency of interventions, it is possible to achieve a pronounced anti-inflammatory, analgesic effect, as well as improve microcirculation, accelerate the elimination of local edema, muscle spasms, etc. Physiotherapy significantly increases the effectiveness of other methods of treatment, but it is mainly used only after the elimination of acute interventionsprocess.
Most often patients are prescribed:
- electrophoresis;
- UHF;
- ultrasound therapy;
- magnetic field therapy;
- reflexology;
- diadynamic currents etc.
A process usually comprises 8-10 sessions that are carried out at regular intervals.
Manual therapy
For osteochondrosis, scoliosis and a number of other diseases, manual therapy sessions can have a really amazing effect on the condition of the spine. But only a qualified chiropractor can competently conduct a manual therapy session and benefit, not harm, the patient.
The use of special techniques of manual manipulation allows not only to improve microcirculation, to relax excessively tight and overly relaxed muscles, but also to increase the distance between the vertebrae and normalize their position. A qualified chiropractor can find the area where the nerve is pinched and relieve the pressure of the anatomical structures on it.

Literally after the first session, the majority of patients notice an improvement in their well-being and a significant decrease in the severity of the pain syndrome until it is completely eliminated. To consolidate the results obtained, it is recommended to undergo full manual therapy and take supportive courses in the future.
Movement therapy
Physiotherapy helps the body deal with the stress. A special series of exercises has been developed for each illness, the regular implementation of which allows the solution of the most important tasks in the current situation. So, with the help of a correctly selected complex of physical therapy exercises, it is possible to restore the muscles to normal tone and strengthen them. Thanks to this, the spine is less stressed, which is an effective prevention of the progression of the disease and creates favorable conditions for its recovery.
Exercise therapy also helps improve blood circulation in the affected area, which speeds up the course of inflammatory processes and is more likely to lead to a full recovery. Proper exercise for many conditions can help reduce back pain and reduce the frequency of its occurrence.
The training program is developed individually for each patient. This takes into account not only the type of pathology detected and the degree of its severity, but also the presence of concomitant diseases, the patient's physical fitness, age and other factors. Only a specialist can correctly choose the most effective and safe exercises.
The first courses take place under his supervision. Meanwhile, the patient learns to correctly perform each suggested exercise so that it is beneficial. Gradually, the load is increased and brought to the optimal level. However, it is not recommended to increase or complicate the number of repetitions of exercises yourself. Changes in the program of physical therapy exercises are made only by a specialist.
The patient just needs to follow his recommendations exactly and practice daily in a comfortable environment. All exercises are done slowly. Sudden movements are not allowed. However, if pain occurs during the class, the exercise should be stopped immediately and you should consult your doctor as soon as possible.
Operation for back pain
Most often, the help of a spinal surgeon is needed with intervertebral hernias, the formation of which has led to an injury to the spine root and the development of radicular pain. If the protrusion has already formed, it cannot be withdrawn using modern non-invasive methods. The only way to get rid of it and get rid of the lower back pain at the same time is to have the intervertebral hernia removed through surgery.

There are different types of operations that are used on intervertebral hernias. The specific tactics of the surgical procedure are determined based on the type, location and size of the hernia:
- Nucleoplasty and hydroplasty are methods of percutaneous surgery in which a portion of the nucleus pulposus can be removed through a puncture of tissues several centimeters in diameter and the size of the hernia reduced.
- Microdiscectomy is a radical way to solve the problem of an intervertebral hernia, in which it or the entire disc is removed through an incision up to 3 cm long. However, unlike other methods, you can get rid of a hernia of any size regardless of its location in the spinal canal, releasing a trapped nerve even in the most difficult part of the spine.
- Endoscopic surgery - involves the removal of a herniated disc through punctures up to 1 cm in diameter using special equipment with a video camera. It can be used to resect hernias of any size, but the technique cannot be used to remove neoplasia in anatomically difficult locations.
With scoliosis, the help of a spinal surgeon is also needed. In this case, all forces are directed towards restoring the normal axis of the spine. Before that, a large incision was required that ran across practically the entire back. However, today it is possible to correct the deformity of the spine through miniature incisions in a minimally invasive way.
Different types of metal structures are used to restore the normal axis of the spine, but their essence is roughly the same. The structure is attached to the vertebrae with special screws. By correcting the tension in different places, it is possible to bring the displaced vertebrae back into place and fix them in the correct position. Modern types of metal structures, over time, make it possible to improve the initial result of the operation without again intervening in the body. This is achieved by correcting the position of the installed structure with special screws.
Surgical intervention cannot be avoided in the case of spinal fractures. In such situations, back pain and back pain can only be eliminated by restoring the vertebrae to normal shape, size and position. For this purpose, kyphoplasty and vertebroplasty have recently been performed. The essence of both operations is based on the fact that a special bone cement is injected into the vertebra through a thin puncture needle, which was destroyed as a result of an injury.  It fills the entire free space and hardens after 10 minutes. However, for severe compression fractures, kyphoplasty is preferred because it can also help restore the vertebra to its normal shape, thereby ensuring the correct distribution of the load on the spine in the future and reducing the risk of complications. This operation involves the preliminary insertion of a special balloon into the destroyed vertebra, which is gradually inflated and returns the vertebra to its original appearance. The balloon is then lowered and removed, and the cavity formed is filled with bone cement.
It fills the entire free space and hardens after 10 minutes. However, for severe compression fractures, kyphoplasty is preferred because it can also help restore the vertebra to its normal shape, thereby ensuring the correct distribution of the load on the spine in the future and reducing the risk of complications. This operation involves the preliminary insertion of a special balloon into the destroyed vertebra, which is gradually inflated and returns the vertebra to its original appearance. The balloon is then lowered and removed, and the cavity formed is filled with bone cement.
Back pain can therefore be the result of physiological changes, frequent muscle fatigue, or a symptom of serious diseases of the spine or internal organs. Therefore, if they appear regularly, and especially against the background of the action of the same factors, then do not hesitate and ignore the problem. Contact qualified specialists so that treatment is as quick and easy as possible. And if the disease could not be detected in the early stages of development, then the modern level of neurosurgery will make it possible to get rid of it surgically with a minimal risk of complications.





































